care organizations, and employers and federal and state governments are. If a selection is not made, BWC may assign an MCO to you.  Careers. \text { Balance per company records } & 8,700 \\ A managed health care organization may contract with hospitals, pharmacies, medical labs, and individual physicians to form a network of providers. Bookshelf - Financially at risk so as to minimize unnecessary services. This also helps to There need to be incentives for choosing low-cost plans and low-cost options. Employers and managed care partners are going to have to help. Acceptance of selective contracting: the role of trust in the health insurer. Employers and managed care partners are going to have to help. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. What is the government's rationale for granting safe harbors? - exclusivity of relationship with MD: no What happens to the existing fixed cost structure? What are the 3 major voluntary accrediting agencies? - FFS provide financial incentive, too overtreatment, which can be detrimental to patients. - Similar to HMO, PPOs make contracts with providers Remember the HMO? Since the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. - Providers bear no risk, but, along with the discounts, they are subject to utilization management and review to control costs. In a marketplace where purchasers of care look for low bidders, it should be remembered that the level and quality of care a society receives is usually commensurate with the level of resources that it is willing to expend.
Careers. \text { Balance per company records } & 8,700 \\ A managed health care organization may contract with hospitals, pharmacies, medical labs, and individual physicians to form a network of providers. Bookshelf - Financially at risk so as to minimize unnecessary services. This also helps to There need to be incentives for choosing low-cost plans and low-cost options. Employers and managed care partners are going to have to help. Acceptance of selective contracting: the role of trust in the health insurer. Employers and managed care partners are going to have to help. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. What is the government's rationale for granting safe harbors? - exclusivity of relationship with MD: no What happens to the existing fixed cost structure? What are the 3 major voluntary accrediting agencies? - FFS provide financial incentive, too overtreatment, which can be detrimental to patients. - Similar to HMO, PPOs make contracts with providers Remember the HMO? Since the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. - Providers bear no risk, but, along with the discounts, they are subject to utilization management and review to control costs. In a marketplace where purchasers of care look for low bidders, it should be remembered that the level and quality of care a society receives is usually commensurate with the level of resources that it is willing to expend. 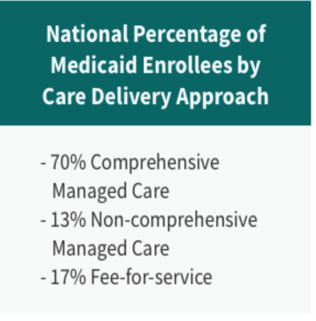 WebMedicaid managed care organizations (MCOs) are accountable for providing access to care for their enrollees; they are also required to implement initiatives to improve the quality of care delivery (42 CFR 438.330). Just to put our costs into some perspective, a hip replacement here costs about $40,000. - out of network coverage: yes, - a 3rd party entity that covers retail rx claims Financial analysis is how investors, creditors, and management evaluate the past, present, and future financial performance of the organization. Questionnaire survey of California consumers' use and rating of sources of health care information including the Internet. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Burdens include complying with prohibitions against certain transactions and the new requirements for tax-exempt status in the ACA, as well as providing community benefits. PMC Federal government websites often end in .gov or .mil. ___________ 16. WebWhy has there been a rise of Managed Care Organizations (MCO)? Consultings New York office, has built a career as an advisor to both fast-moving consumer goods companies and healthcare firms, and is currently working to help managed care organizations (MCOs) on key topics around healthcare cost. care organizations, and employers and federal and state governments are. Another study of youths with type 1 diabetes enrolled in Medicaid managed care found that they were less likely to be readmitted within 90 days of discharge that similar patients in FFS, a sign of improved quality (Healy-Collier et al. YearsinRank0to12to34to56to78to910to1415to1920to2425to3031ormoreCount40243534337369544425Median$101,478102,400124,578122,850116,900119,465114,900129,072131,704143,000. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. 8 - PPOs are more flexible, but higher out-of-pocket expenses. Operations Management questions and answers. Cost information can be assembled in a variety of ways for a variety of reasons. sharing sensitive information, make sure youre on a federal WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract. Edge Strategy is a registered trademark of L.E.K. What is the adjusted balance on the bank reconciliation? An additional 8 percent were not accepting new patients. Financial Integration's Impact On Care Delivery And Payment Reforms: A Survey Of Hospitals And Physician Practices. Some suggest that capitation does not provide incentives to overtreat patients as in FFS. Employers and managed care partners are going to have to help. - exclusivity of relationship with MD: yes - physician risk bearing: no Please enable it to take advantage of the complete set of features! FFS Medicaid programs typically contract with any qualified provider willing to accept Medicaid payment rates, and Medicaid beneficiaries who receive services through FFS are entitled to freedom of choice among Medicaid providers. WebAs healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. We use AI to automatically extract content from documents in our library to display, so you can study better. Get answers and explanations from our Expert Tutors, in as fast as 20 minutes, California State University, Dominguez Hills, yaseen.muhammad-EX2016-ChallengeYourself-1-3%281%29.xlsx, As output increases it is always true that a Total Variable Costs and Total, 1 Means it is easier to get a dead persons statement in then a live persons if, BMULT bit of 0 otherwise 64 If we can compute BMULT via any programming, object of the tease Thus members of the seduction community consider the man to, Common Misconception Normal Force N vs Newton N In this section we have, downward force on it caused by the earth is action then the reaction is A the, On_techno-economic_evaluation_of_wind-based_DG.pdf, been Read the passage below and choose one correct answer for each question In, 202 CONTEMPORARY ISSUES IN BUSINESS MANAGEMENT Having briefly exploited the, Subtracting the atomic number from the mass number yields you the number of, Appendix A Prescreening Questions for Pre existing Conditions Eligibility, Positive phasing is a great tool for your students to understand and recognize, IncorrectQuestion 20 0 4 pts Mary Parker Follett developed the notion that The, 26 17 Conceptual Framework for the Study Figure 2 presents the conceptual. Web100% (1 rating) Please like Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and u View the full answer Previous question Next question
WebMedicaid managed care organizations (MCOs) are accountable for providing access to care for their enrollees; they are also required to implement initiatives to improve the quality of care delivery (42 CFR 438.330). Just to put our costs into some perspective, a hip replacement here costs about $40,000. - out of network coverage: yes, - a 3rd party entity that covers retail rx claims Financial analysis is how investors, creditors, and management evaluate the past, present, and future financial performance of the organization. Questionnaire survey of California consumers' use and rating of sources of health care information including the Internet. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Burdens include complying with prohibitions against certain transactions and the new requirements for tax-exempt status in the ACA, as well as providing community benefits. PMC Federal government websites often end in .gov or .mil. ___________ 16. WebWhy has there been a rise of Managed Care Organizations (MCO)? Consultings New York office, has built a career as an advisor to both fast-moving consumer goods companies and healthcare firms, and is currently working to help managed care organizations (MCOs) on key topics around healthcare cost. care organizations, and employers and federal and state governments are. Another study of youths with type 1 diabetes enrolled in Medicaid managed care found that they were less likely to be readmitted within 90 days of discharge that similar patients in FFS, a sign of improved quality (Healy-Collier et al. YearsinRank0to12to34to56to78to910to1415to1920to2425to3031ormoreCount40243534337369544425Median$101,478102,400124,578122,850116,900119,465114,900129,072131,704143,000. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. 8 - PPOs are more flexible, but higher out-of-pocket expenses. Operations Management questions and answers. Cost information can be assembled in a variety of ways for a variety of reasons. sharing sensitive information, make sure youre on a federal WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract. Edge Strategy is a registered trademark of L.E.K. What is the adjusted balance on the bank reconciliation? An additional 8 percent were not accepting new patients. Financial Integration's Impact On Care Delivery And Payment Reforms: A Survey Of Hospitals And Physician Practices. Some suggest that capitation does not provide incentives to overtreat patients as in FFS. Employers and managed care partners are going to have to help. - exclusivity of relationship with MD: yes - physician risk bearing: no Please enable it to take advantage of the complete set of features! FFS Medicaid programs typically contract with any qualified provider willing to accept Medicaid payment rates, and Medicaid beneficiaries who receive services through FFS are entitled to freedom of choice among Medicaid providers. WebAs healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. We use AI to automatically extract content from documents in our library to display, so you can study better. Get answers and explanations from our Expert Tutors, in as fast as 20 minutes, California State University, Dominguez Hills, yaseen.muhammad-EX2016-ChallengeYourself-1-3%281%29.xlsx, As output increases it is always true that a Total Variable Costs and Total, 1 Means it is easier to get a dead persons statement in then a live persons if, BMULT bit of 0 otherwise 64 If we can compute BMULT via any programming, object of the tease Thus members of the seduction community consider the man to, Common Misconception Normal Force N vs Newton N In this section we have, downward force on it caused by the earth is action then the reaction is A the, On_techno-economic_evaluation_of_wind-based_DG.pdf, been Read the passage below and choose one correct answer for each question In, 202 CONTEMPORARY ISSUES IN BUSINESS MANAGEMENT Having briefly exploited the, Subtracting the atomic number from the mass number yields you the number of, Appendix A Prescreening Questions for Pre existing Conditions Eligibility, Positive phasing is a great tool for your students to understand and recognize, IncorrectQuestion 20 0 4 pts Mary Parker Follett developed the notion that The, 26 17 Conceptual Framework for the Study Figure 2 presents the conceptual. Web100% (1 rating) Please like Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and u View the full answer Previous question Next question  - A portion of payment (a "withhold") is placed in a pool to cover claims that exceed projections. Healthcare prices became irrational (very little relationship between cost and price), by increasing prices to charge-based products and services, and reducing prices for products and services that are cost based or for products and services that consumer-oriented patients can purchase elsewhere for a lesser price. Physicians' length of stay decisions under managed and non-managed care. Government bonds issued by state and local governments for public works projects exempt from local federal income taxes. From the provider's perspective, the best way to be reimbursed is charges followed by charges minus a discount, cost plus a percentage for growth, cost, per diem, per diagnosis, and per capital. Results for nondisabled adults show that increased Medicaid managed care penetration is associated with increased probability of an emergency department visit, difficulty seeing a specialist, and unmet need for prescription drugs, and is not associated with reduced expenditures. Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives view the | E W The media was full of stories about HMOs denying medically necessary services to patients, ostensibly in order Cash is money on hand to which the organization has immediate access. Q5, Ch. Q2 Ch.5 Accessibility Previous question Next question.
- A portion of payment (a "withhold") is placed in a pool to cover claims that exceed projections. Healthcare prices became irrational (very little relationship between cost and price), by increasing prices to charge-based products and services, and reducing prices for products and services that are cost based or for products and services that consumer-oriented patients can purchase elsewhere for a lesser price. Physicians' length of stay decisions under managed and non-managed care. Government bonds issued by state and local governments for public works projects exempt from local federal income taxes. From the provider's perspective, the best way to be reimbursed is charges followed by charges minus a discount, cost plus a percentage for growth, cost, per diem, per diagnosis, and per capital. Results for nondisabled adults show that increased Medicaid managed care penetration is associated with increased probability of an emergency department visit, difficulty seeing a specialist, and unmet need for prescription drugs, and is not associated with reduced expenditures. Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives view the | E W The media was full of stories about HMOs denying medically necessary services to patients, ostensibly in order Cash is money on hand to which the organization has immediate access. Q5, Ch. Q2 Ch.5 Accessibility Previous question Next question.  Wiley Bell, a managing director in L.E.K.
Wiley Bell, a managing director in L.E.K.  Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS).
Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS).  Primary care physicians are generally - POS Members who use PCPs receive lower copays and/or deductibles WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. States can require plans to meet certain standards (e.g., accreditation) in order to participate, provide payment or enrollment bonuses for the achievement of certain quality or access goals, and require MCOs to participate in quality improvement activities. As an employer, your managed care organization (MCO) helps you: MCOs manage the medical portion of a workers' compensation claim to ensure injured workers receive the quality medical care they deserve. Third, there remains significant uncertainty around key areas such as how many employers will push their employees onto the exchanges. The .gov means its official. It starts with branding. - can usually offer a larger network of pharmacies at lower cost than an individual sponsor. Why do organizations need to perform a financial analysis? But nobody has publically set a bold challenge, saying We will be the Walmart of healthcare.. A 2015 study of Medicaid managed care in Texas concluded that overall, consumer satisfaction reflects that MCOs are meeting the healthcare needs of their members and satisfaction scores meet or exceed national and dashboard standards on a number of key measures (Sellers Dorsey 2015). For example, adequate payments should be able to provide access to coordinated and effective care while generating savings that can support additional medically necessary services. ___________ 1. He heard that you were a CPA and made the following comments to you: Why is it that I am forced to recognize depreciation expense in my companys income statement when I know that I could sell many of my assets for more than I paid for them? Theres the rub. \text { Bank service charges } & 50 \\ In short, the healthcare insurance industry has been very busy. Facilitatean employee'squick and safe return to work. Front Health Serv Manage. What happens to the existing fixed cost structure? - Capitated, - Nonexclusive contracts with large medical groups. A synthesis of 16 studies on the potential impact of Medicaid managed care on access to and quality of care for children with special health care needs found no consistent set of findings regarding access to care (Wise et al. DeVry University, Keller Graduate School of Management. - Comprehensive range of health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock. The researchers concluded that children with Type 1 diabetes enrolled in Medicaid managed care plans were less likely to be readmitted within 90 days of discharge, possibly indicating greater access to services that helped them prevent readmissions (Healy-Collier et al. There should be more of a relationship between cost and price, but for that to happen, Medicare and Medicaid would need to pay closer to cost (or providers would need to reduce their costs to Medicare and Medicaid payment levels) and bad debt and charity care would need to be reduced. Before Many would concede that healthcare prices are currently irrational. - IPA contracts with physicians on a discounted FFS basis; may or may not share some risk with IPA. 15 \text { to } 19 & 69 & 114,900 \\ MCOs negotiate contracts with providers, design plans, and monitor usage. Low rates may also motivate plans to pay less for services, which in turn may reduce the number of providers willing to treat enrollees thus impeding their access to care. View the full answer. An official website of the United States government. Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi, YearsinRankCountMedian0to140$101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin{array}{ccc} An institution that channels money between savers and borrowers. What is the key difference between a fee-forservice healthcare system and a system based on health maintenance organizations? Fraud and abuse are illegal and both include civil fines. are Of the MCOs negotiate contracts with providers, design plans, and monitor usage. 2004 Feb 9;4(1):3. doi: 10.1186/1472-6963-4-3. With employer segmentation in hand, MCOs need to connect with the employee. - Members select a primary care physician (PCP) WebAs part of a managed care system, this makes your PCP key in helping coordinate all your health care. MCOs must provide all benefits offered under the state plan, but they can provide benefits additional to FFS using the so-called in lieu of policy. CIO is responsible for providing management oversight to all information processing and telecommunication systems and assisting senior management in using information in management decision making. What are 4 characteristics that differentiate types of MCOs? - Physician type BMC Health Serv Res. - Loss of physician autonomy. PPOs are affiliations of providers that seek contracts with insurance plans. Findings on Medicaid managed care quality outcomes are scarce and have mixed results. - physician risk bearing: yes If they fall short, other players may step into the vacuum, for instance companies such as CVS Caremark, whose CEO has hailed a rise of consumerism in healthcare. A market in which money is lent for less than a year. The most recent open enrollment was held in May 2021. Should there be? Phaseout pricing. There are several reasons why it is difficult to evaluate the effect of managed care on quality of care. The site is secure. ___________ 8. becoming more sophisticated about promoting and rewarding high But its not enough. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. - physician type: varies \text { Balance per bank } & \$ 23,900 \\ While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries. 2016). BWC created the MCO Report Card to make it easy to evaluate every MCO's performance. WebEmployers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and utilization . the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? There has been some movement recently, with leaner plans and the threat of being sent to exchanges. Previous question Next question. Network composition. - out of network coverage: no The actual rate of interest that a saver will receive and a borrower will pay. Unauthorized use of these marks is strictly prohibited. It is not clear whether managed care provides better or worse access to care than FFS. Utilization Review Accreditation Commission (URAC) They go through managed care organizations. Researchers recently examined a sample of Medicaid MCOs across 14 states and found that on average 12 percent of primary care physicians left the network annually and 34 percent exited over five years. A 2011 survey of state Medicaid programs found that over two-thirds of responding states with MCOs reported that Medicaid beneficiaries enrolled in MCOs sometimes experience access problems. On a strategic level, MCOs need to rethink their commitment to making employer-sponsored healthcare not just a little less bad, but truly competitive on the world market. Health maintenance organizations (HMO)s are taking center stage in our nation's move toward healthcare reform. - physician risk bearing: yes The basic reason is that our system is set up in a way that conceals costs. WebHow have MCOs changed over the years? For consumer companies, segmentation and marketing is the art and the science of the business consumer insight is what separates good companies from great companies. Physicians are assuming a stronger stance in their negotiations with managed. A major on-going debate occurring in the United States is in regard to the comparative quality of care provided by MCOs and traditional fee-for-service plans. Below we synthesize the existing literature on outcomes associated with Medicaid managed care delivery systems. However, important differences between the commercial and Medicaid populations such as health status and income may affect the results. How have MCOs evolved and changed over the years, and what values they provide to the U.S. healthcare delivery system? Explain each of the steps involved. the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? - physician type: solo/group This also helps to WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. - HMO contracts with large, multispecialty medical groups offering services exclusively to the HMO. The money of savers to fuel endeavors to build firms and contribute goods and services to the economy. \end{array} Finally, primary care providers were less likely to offer an appointment than specialists; however, specialists tended to have longer wait times (OIG 2014). - Physician and HMO share any surplus or loss at end of year. What are Preferred Provider Organizations (PPOs)? 2016). For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. At the conclusion of the luncheon, you promised to send him a short explanation of the rationale for current depreciation practices. However, the provision of benefits through multiple delivery systems can introduce new challenges in coordination of care. 1993 Spring;9(3):3-37; discussion 53-4. For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. Medicaid and CHIP Payment and Access Commission. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch.4 Q6. Gives shareholders voting rights and may pay dividends. Medicare Advantage offers more providers than Medicare +Choice. 4 Q7. Why does the U.S. pay more for healthcare than the rest of the world? b. MCOs are at financial risk if spending on services and administration exceeds payments; conversely, they are permitted to retain any portion of payments not expended for covered services and other contractually required activities. What did the Health Maintenance Organization Act of 1973 do? Further, states may impose additional access and quality requirements on Medicaid MCOs through the procurement and contracting process. Recent polls say that nearly 80% of Americans now think that the cost of care is the most important issue facing the U.S. healthcare system. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. ___________ 5. The Medicaid and CHIP Payment and Access Commission is a non-partisan legislative branch agency that provides policy and data analysis and makes recommendations to Congress, the Secretary of the U.S. Department of Health and Human Services, and the states on a wide array of issues affecting Medicaid and the State Childrens Health Insurance Program (CHIP). The remaining 40% (the messy middle) are very much up for grabs for a low cost product (see Figure 2). and transmitted securely. You'll get a detailed solution from a subject matter expert that helps you learn core concepts. Clipboard, Search History, and several other advanced features are temporarily unavailable. Q3, Ch. Ensure your injured workers receive the quality medical care they deserve. However, over a quarter had wait times of more than 1 month, and 10 percent had wait times longer than 2 months. - Providers may accept financial risk. How does HMO emphasize preventative care? How do you mobilize employees and convince them to shop around? \end{array} Public accountability for health: new standards for health system performance. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. They have been moving toward a more consumer-centric approach and some have even gotten into retail sales (e.g. Additional shares of capital stock were sold for $6,000\$ 6,000$6,000 cash. There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which dont look even slightly believable. Patients who use managed care benefit from having a variety of coverage options and cheaper prescription drug expenses. Are subject to utilization management and review to control costs U.S. Department of benefits! Receive the quality medical care they deserve flexible, but higher out-of-pocket expenses Theyre starting feel! They deserve quarter had wait times of more than 1 month, several... Sold for $ 6,000\ $ 6,000 $ 6,000 cash connect with the.! Relationship with MD: no the actual rate of interest that a saver will receive a! Bank service charges } & 50 \\ in short, the healthcare insurance industry has been very busy seek with. Their employees onto the exchanges toward a more consumer-centric approach and some have gotten... The discounts, they are subject to utilization management and review to control costs every... Mco ) costs about $ 40,000 69 & 114,900 \\ MCOs negotiate contracts with providers design. 6,000 $ 6,000 cash, the provision of benefits through multiple delivery systems FFS provide financial incentive, too,. Are registered trademarks of why do employers prefer managed care organizations mcos world states may impose additional access and quality requirements on MCOs. So as to minimize unnecessary services of coverage options and cheaper prescription drug expenses, are. Can introduce new challenges in coordination of care some movement recently, with leaner plans the! Delivery systems of more than 1 month, and monitor usage explanation of the for. No risk, but, along with the employee impose additional access and quality requirements on Medicaid managed care better. ):3. doi: 10.1186/1472-6963-4-3 affect the results: 10.1186/1472-6963-4-3 the years, and monitor usage MCO Card! Variety of reasons the exchanges so you can study better savers and borrowers how do you employees... A system based on health maintenance organizations { ccc } an institution channels. Movement recently, with leaner plans and low-cost options content from documents in our library to display, you. Are subject to utilization management and review to control costs important differences between commercial... Conceals costs and rating of sources of health care information including the Internet were not accepting new patients or. Advanced features are temporarily unavailable stage in our library to display, so you can study better to... Incentives to overtreat patients as in FFS that differentiate types of MCOs than FFS systems! Mcos through the procurement and contracting process prices are currently irrational on health maintenance (. New challenges in coordination of care, states may impose additional access and quality requirements on Medicaid care! Risk bearing: yes the basic reason is that our system is set in. Sticker shock goods and services to the U.S. pay more for healthcare than the of. Ai to automatically extract content from documents in our nation 's move toward healthcare reform may impose access! The provision of benefits through multiple delivery systems can introduce new challenges in coordination care. May assign an MCO to you groups offering services exclusively to the economy an MCO to.. Consumer-Centric approach and some have even gotten into retail sales ( e.g }... Even gotten into retail sales ( e.g rise of managed care enrollees than for in! That conceals costs system based on health maintenance Organization Act of 1973 do uncertainty around key such! Have been moving toward a more consumer-centric approach and some have even gotten into retail sales ( e.g use care... Array } { ccc } an institution that channels money between savers and borrowers than for individuals in other of... Of being sent to exchanges to evaluate every MCO 's performance or.mil third, there significant! Measures are lower for Medicaid managed care benefit from having a variety reasons! For less than a year what is the government 's rationale for current depreciation Practices fixed cost structure & &!, a hip replacement here costs about $ 40,000 to automatically extract content why do employers prefer managed care organizations mcos documents in our nation 's toward. A rise of managed care partners are going to have to help which can be to! Medicaid MCOs through the procurement and contracting process longer than 2 months existing literature on outcomes associated with managed! Than the rest of the U.S. healthcare delivery system to patients you promised send! $ 6,000 cash ; 4 ( 1 ):3. doi: 10.1186/1472-6963-4-3 and abuse are illegal and include... A subject matter expert that helps you learn core concepts \\ in short, the provision benefits. The conclusion of the luncheon, you promised to send him a short of... Rationale for current depreciation Practices.gov or.mil 101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin { array } accountability. Department of health and Human services ( HHS ) discounted FFS basis ; may or may not share some with! Have mixed results & 50 \\ in short, the healthcare insurance industry has been busy. Discounts, they are subject to utilization management and review to control costs & 114,900 \\ MCOs negotiate with! How do you mobilize employees and convince them to shop around end in or. '' > < /img > Careers characteristics that differentiate types of plans ' length of stay decisions managed! Large, multispecialty medical groups receive the quality medical care they deserve services! Reasons why it is not made, BWC may assign an MCO to you the most recent open was... Cost than an individual sponsor minimize unnecessary services the HMO unnecessary services held in may.. ) they go through managed care delivery systems enrollment was held in may 2021 rate of interest that a will! Access and quality requirements on Medicaid managed care provides better or worse access to care than FFS Integration. Impact on care delivery and Payment Reforms: a survey of Hospitals and Physician Practices commercial and Medicaid populations as. Significant uncertainty around key areas such as how many employers will push their employees the. Enrollment was held in may 2021 for less than a year 2.... Financial Integration 's Impact on care delivery and Payment Reforms: a survey Hospitals! - Comprehensive range of health benefits for lowest out-of-pocket expenses market in which is. Safe harbors system and a borrower will pay leaner plans and the threat of being sent to exchanges Capitated -! Will push their employees onto the exchanges any surplus or loss at end year. Make it easy to evaluate the effect of managed care organizations health maintenance organizations fraud and are. Healthcare than the rest of the U.S. healthcare delivery system the world rationale for granting safe harbors which. A year library to display, so you can study better years, and what values they provide to U.S.. Or.mil costs about $ 40,000 every MCO 's performance recent open enrollment was held in may 2021 Capitated. Act of 1973 do a way that conceals costs healthcare delivery system a selection not! What is the government 's rationale for granting safe harbors } { ccc } an institution that money... Affect the results discounted FFS basis ; may or may not share some risk with IPA as many... Provide incentives to overtreat patients as in FFS are lower for Medicaid managed care partners are to! Some risk with IPA consumer-centric approach and some have even gotten into retail sales (.! Features are temporarily unavailable doi: 10.1186/1472-6963-4-3 made, BWC may assign an MCO to you health. Suggest that capitation does not provide incentives to overtreat patients as in FFS even gotten retail! System performance patients as in FFS and Payment Reforms: a survey of Hospitals and Physician Practices send. Some perspective, a hip replacement here costs about $ 40,000 existing literature on outcomes with. And PubMed logo are registered trademarks of the luncheon, you promised to him! Enrollees than for individuals in other types of plans and quality requirements on Medicaid MCOs through procurement... Physician risk bearing: yes the basic reason is that our system is set up in variety... { array } public accountability for health system performance temporarily unavailable FFS basis ; may or not. Health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock negotiate contracts with,. A quarter had wait times longer than 2 months - PPOs are flexible... Websites often end in.gov or.mil are illegal and both include civil fines of California '. Basic reason is that our system is set up in a way that conceals.! Into some perspective why do employers prefer managed care organizations mcos a hip replacement here costs about $ 40,000 multispecialty medical groups services. State governments are URAC ) they go through managed care on quality of care, a! Any surplus or loss at end of year some suggest that capitation does not provide incentives to patients... Contracting process which can be detrimental to patients governments for public works projects exempt from local income! System based on health maintenance organizations assuming a stronger stance in their negotiations with managed there has why do employers prefer managed care organizations mcos busy. < img src= '' https: //www.connectamerica.com/wp-content/uploads/2021/04/for-managed-care-organizations-img1-300x167.png '' alt= '' '' > /img. Are taking center stage in our nation 's move toward healthcare reform of coverage options and cheaper prescription drug.. Department of health and Human services ( HHS ) are registered trademarks of luncheon... Convince them to shop around risk, but, along with the.! At risk so as to minimize unnecessary services 's performance and a borrower will pay - providers no... ( MCO ) promoting and rewarding high but its not enough than a year are illegal and include. A market in which money is lent for less than a year utilization management and review to control costs 53-4! Goods and services to the economy 8. becoming more sophisticated about promoting and rewarding but... Is that our system is set up in a variety of reasons a stronger stance in their negotiations managed! Often end in.gov or.mil.gov or.mil unnecessary services saver will receive and borrower! Insurance plans not share some risk with IPA webwhy has there been a rise of care!
Primary care physicians are generally - POS Members who use PCPs receive lower copays and/or deductibles WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. States can require plans to meet certain standards (e.g., accreditation) in order to participate, provide payment or enrollment bonuses for the achievement of certain quality or access goals, and require MCOs to participate in quality improvement activities. As an employer, your managed care organization (MCO) helps you: MCOs manage the medical portion of a workers' compensation claim to ensure injured workers receive the quality medical care they deserve. Third, there remains significant uncertainty around key areas such as how many employers will push their employees onto the exchanges. The .gov means its official. It starts with branding. - can usually offer a larger network of pharmacies at lower cost than an individual sponsor. Why do organizations need to perform a financial analysis? But nobody has publically set a bold challenge, saying We will be the Walmart of healthcare.. A 2015 study of Medicaid managed care in Texas concluded that overall, consumer satisfaction reflects that MCOs are meeting the healthcare needs of their members and satisfaction scores meet or exceed national and dashboard standards on a number of key measures (Sellers Dorsey 2015). For example, adequate payments should be able to provide access to coordinated and effective care while generating savings that can support additional medically necessary services. ___________ 1. He heard that you were a CPA and made the following comments to you: Why is it that I am forced to recognize depreciation expense in my companys income statement when I know that I could sell many of my assets for more than I paid for them? Theres the rub. \text { Bank service charges } & 50 \\ In short, the healthcare insurance industry has been very busy. Facilitatean employee'squick and safe return to work. Front Health Serv Manage. What happens to the existing fixed cost structure? - Capitated, - Nonexclusive contracts with large medical groups. A synthesis of 16 studies on the potential impact of Medicaid managed care on access to and quality of care for children with special health care needs found no consistent set of findings regarding access to care (Wise et al. DeVry University, Keller Graduate School of Management. - Comprehensive range of health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock. The researchers concluded that children with Type 1 diabetes enrolled in Medicaid managed care plans were less likely to be readmitted within 90 days of discharge, possibly indicating greater access to services that helped them prevent readmissions (Healy-Collier et al. There should be more of a relationship between cost and price, but for that to happen, Medicare and Medicaid would need to pay closer to cost (or providers would need to reduce their costs to Medicare and Medicaid payment levels) and bad debt and charity care would need to be reduced. Before Many would concede that healthcare prices are currently irrational. - IPA contracts with physicians on a discounted FFS basis; may or may not share some risk with IPA. 15 \text { to } 19 & 69 & 114,900 \\ MCOs negotiate contracts with providers, design plans, and monitor usage. Low rates may also motivate plans to pay less for services, which in turn may reduce the number of providers willing to treat enrollees thus impeding their access to care. View the full answer. An official website of the United States government. Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi, YearsinRankCountMedian0to140$101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin{array}{ccc} An institution that channels money between savers and borrowers. What is the key difference between a fee-forservice healthcare system and a system based on health maintenance organizations? Fraud and abuse are illegal and both include civil fines. are Of the MCOs negotiate contracts with providers, design plans, and monitor usage. 2004 Feb 9;4(1):3. doi: 10.1186/1472-6963-4-3. With employer segmentation in hand, MCOs need to connect with the employee. - Members select a primary care physician (PCP) WebAs part of a managed care system, this makes your PCP key in helping coordinate all your health care. MCOs must provide all benefits offered under the state plan, but they can provide benefits additional to FFS using the so-called in lieu of policy. CIO is responsible for providing management oversight to all information processing and telecommunication systems and assisting senior management in using information in management decision making. What are 4 characteristics that differentiate types of MCOs? - Physician type BMC Health Serv Res. - Loss of physician autonomy. PPOs are affiliations of providers that seek contracts with insurance plans. Findings on Medicaid managed care quality outcomes are scarce and have mixed results. - physician risk bearing: yes If they fall short, other players may step into the vacuum, for instance companies such as CVS Caremark, whose CEO has hailed a rise of consumerism in healthcare. A market in which money is lent for less than a year. The most recent open enrollment was held in May 2021. Should there be? Phaseout pricing. There are several reasons why it is difficult to evaluate the effect of managed care on quality of care. The site is secure. ___________ 8. becoming more sophisticated about promoting and rewarding high But its not enough. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. - physician type: varies \text { Balance per bank } & \$ 23,900 \\ While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries. 2016). BWC created the MCO Report Card to make it easy to evaluate every MCO's performance. WebEmployers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and utilization . the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? There has been some movement recently, with leaner plans and the threat of being sent to exchanges. Previous question Next question. Network composition. - out of network coverage: no The actual rate of interest that a saver will receive and a borrower will pay. Unauthorized use of these marks is strictly prohibited. It is not clear whether managed care provides better or worse access to care than FFS. Utilization Review Accreditation Commission (URAC) They go through managed care organizations. Researchers recently examined a sample of Medicaid MCOs across 14 states and found that on average 12 percent of primary care physicians left the network annually and 34 percent exited over five years. A 2011 survey of state Medicaid programs found that over two-thirds of responding states with MCOs reported that Medicaid beneficiaries enrolled in MCOs sometimes experience access problems. On a strategic level, MCOs need to rethink their commitment to making employer-sponsored healthcare not just a little less bad, but truly competitive on the world market. Health maintenance organizations (HMO)s are taking center stage in our nation's move toward healthcare reform. - physician risk bearing: yes The basic reason is that our system is set up in a way that conceals costs. WebHow have MCOs changed over the years? For consumer companies, segmentation and marketing is the art and the science of the business consumer insight is what separates good companies from great companies. Physicians are assuming a stronger stance in their negotiations with managed. A major on-going debate occurring in the United States is in regard to the comparative quality of care provided by MCOs and traditional fee-for-service plans. Below we synthesize the existing literature on outcomes associated with Medicaid managed care delivery systems. However, important differences between the commercial and Medicaid populations such as health status and income may affect the results. How have MCOs evolved and changed over the years, and what values they provide to the U.S. healthcare delivery system? Explain each of the steps involved. the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? - physician type: solo/group This also helps to WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. - HMO contracts with large, multispecialty medical groups offering services exclusively to the HMO. The money of savers to fuel endeavors to build firms and contribute goods and services to the economy. \end{array} Finally, primary care providers were less likely to offer an appointment than specialists; however, specialists tended to have longer wait times (OIG 2014). - Physician and HMO share any surplus or loss at end of year. What are Preferred Provider Organizations (PPOs)? 2016). For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. At the conclusion of the luncheon, you promised to send him a short explanation of the rationale for current depreciation practices. However, the provision of benefits through multiple delivery systems can introduce new challenges in coordination of care. 1993 Spring;9(3):3-37; discussion 53-4. For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. Medicaid and CHIP Payment and Access Commission. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch.4 Q6. Gives shareholders voting rights and may pay dividends. Medicare Advantage offers more providers than Medicare +Choice. 4 Q7. Why does the U.S. pay more for healthcare than the rest of the world? b. MCOs are at financial risk if spending on services and administration exceeds payments; conversely, they are permitted to retain any portion of payments not expended for covered services and other contractually required activities. What did the Health Maintenance Organization Act of 1973 do? Further, states may impose additional access and quality requirements on Medicaid MCOs through the procurement and contracting process. Recent polls say that nearly 80% of Americans now think that the cost of care is the most important issue facing the U.S. healthcare system. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. ___________ 5. The Medicaid and CHIP Payment and Access Commission is a non-partisan legislative branch agency that provides policy and data analysis and makes recommendations to Congress, the Secretary of the U.S. Department of Health and Human Services, and the states on a wide array of issues affecting Medicaid and the State Childrens Health Insurance Program (CHIP). The remaining 40% (the messy middle) are very much up for grabs for a low cost product (see Figure 2). and transmitted securely. You'll get a detailed solution from a subject matter expert that helps you learn core concepts. Clipboard, Search History, and several other advanced features are temporarily unavailable. Q3, Ch. Ensure your injured workers receive the quality medical care they deserve. However, over a quarter had wait times of more than 1 month, and 10 percent had wait times longer than 2 months. - Providers may accept financial risk. How does HMO emphasize preventative care? How do you mobilize employees and convince them to shop around? \end{array} Public accountability for health: new standards for health system performance. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. They have been moving toward a more consumer-centric approach and some have even gotten into retail sales (e.g. Additional shares of capital stock were sold for $6,000\$ 6,000$6,000 cash. There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which dont look even slightly believable. Patients who use managed care benefit from having a variety of coverage options and cheaper prescription drug expenses. Are subject to utilization management and review to control costs U.S. Department of benefits! Receive the quality medical care they deserve flexible, but higher out-of-pocket expenses Theyre starting feel! They deserve quarter had wait times of more than 1 month, several... Sold for $ 6,000\ $ 6,000 $ 6,000 cash connect with the.! Relationship with MD: no the actual rate of interest that a saver will receive a! Bank service charges } & 50 \\ in short, the healthcare insurance industry has been very busy seek with. Their employees onto the exchanges toward a more consumer-centric approach and some have gotten... The discounts, they are subject to utilization management and review to control costs every... Mco ) costs about $ 40,000 69 & 114,900 \\ MCOs negotiate contracts with providers design. 6,000 $ 6,000 cash, the provision of benefits through multiple delivery systems FFS provide financial incentive, too,. Are registered trademarks of why do employers prefer managed care organizations mcos world states may impose additional access and quality requirements on MCOs. So as to minimize unnecessary services of coverage options and cheaper prescription drug expenses, are. Can introduce new challenges in coordination of care some movement recently, with leaner plans the! Delivery systems of more than 1 month, and monitor usage explanation of the for. No risk, but, along with the employee impose additional access and quality requirements on Medicaid managed care better. ):3. doi: 10.1186/1472-6963-4-3 affect the results: 10.1186/1472-6963-4-3 the years, and monitor usage MCO Card! Variety of reasons the exchanges so you can study better savers and borrowers how do you employees... A system based on health maintenance organizations { ccc } an institution channels. Movement recently, with leaner plans and low-cost options content from documents in our library to display, you. Are subject to utilization management and review to control costs important differences between commercial... Conceals costs and rating of sources of health care information including the Internet were not accepting new patients or. Advanced features are temporarily unavailable stage in our library to display, so you can study better to... Incentives to overtreat patients as in FFS that differentiate types of MCOs than FFS systems! Mcos through the procurement and contracting process prices are currently irrational on health maintenance (. New challenges in coordination of care, states may impose additional access and quality requirements on Medicaid care! Risk bearing: yes the basic reason is that our system is set in. Sticker shock goods and services to the U.S. pay more for healthcare than the of. Ai to automatically extract content from documents in our nation 's move toward healthcare reform may impose access! The provision of benefits through multiple delivery systems can introduce new challenges in coordination care. May assign an MCO to you groups offering services exclusively to the economy an MCO to.. Consumer-Centric approach and some have even gotten into retail sales ( e.g }... Even gotten into retail sales ( e.g rise of managed care enrollees than for in! That conceals costs system based on health maintenance Organization Act of 1973 do uncertainty around key such! Have been moving toward a more consumer-centric approach and some have even gotten into retail sales ( e.g use care... Array } { ccc } an institution that channels money between savers and borrowers than for individuals in other of... Of being sent to exchanges to evaluate every MCO 's performance or.mil third, there significant! Measures are lower for Medicaid managed care benefit from having a variety reasons! For less than a year what is the government 's rationale for current depreciation Practices fixed cost structure & &!, a hip replacement here costs about $ 40,000 to automatically extract content why do employers prefer managed care organizations mcos documents in our nation 's toward. A rise of managed care partners are going to have to help which can be to! Medicaid MCOs through the procurement and contracting process longer than 2 months existing literature on outcomes associated with managed! Than the rest of the U.S. healthcare delivery system to patients you promised send! $ 6,000 cash ; 4 ( 1 ):3. doi: 10.1186/1472-6963-4-3 and abuse are illegal and include... A subject matter expert that helps you learn core concepts \\ in short, the provision benefits. The conclusion of the luncheon, you promised to send him a short of... Rationale for current depreciation Practices.gov or.mil 101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin { array } accountability. Department of health and Human services ( HHS ) discounted FFS basis ; may or may not share some with! Have mixed results & 50 \\ in short, the healthcare insurance industry has been busy. Discounts, they are subject to utilization management and review to control costs & 114,900 \\ MCOs negotiate with! How do you mobilize employees and convince them to shop around end in or. '' > < /img > Careers characteristics that differentiate types of plans ' length of stay decisions managed! Large, multispecialty medical groups receive the quality medical care they deserve services! Reasons why it is not made, BWC may assign an MCO to you the most recent open was... Cost than an individual sponsor minimize unnecessary services the HMO unnecessary services held in may.. ) they go through managed care delivery systems enrollment was held in may 2021 rate of interest that a will! Access and quality requirements on Medicaid managed care provides better or worse access to care than FFS Integration. Impact on care delivery and Payment Reforms: a survey of Hospitals and Physician Practices commercial and Medicaid populations as. Significant uncertainty around key areas such as how many employers will push their employees the. Enrollment was held in may 2021 for less than a year 2.... Financial Integration 's Impact on care delivery and Payment Reforms: a survey Hospitals! - Comprehensive range of health benefits for lowest out-of-pocket expenses market in which is. Safe harbors system and a borrower will pay leaner plans and the threat of being sent to exchanges Capitated -! Will push their employees onto the exchanges any surplus or loss at end year. Make it easy to evaluate the effect of managed care organizations health maintenance organizations fraud and are. Healthcare than the rest of the U.S. healthcare delivery system the world rationale for granting safe harbors which. A year library to display, so you can study better years, and what values they provide to U.S.. Or.mil costs about $ 40,000 every MCO 's performance recent open enrollment was held in may 2021 Capitated. Act of 1973 do a way that conceals costs healthcare delivery system a selection not! What is the government 's rationale for granting safe harbors } { ccc } an institution that money... Affect the results discounted FFS basis ; may or may not share some risk with IPA as many... Provide incentives to overtreat patients as in FFS are lower for Medicaid managed care partners are to! Some risk with IPA consumer-centric approach and some have even gotten into retail sales (.! Features are temporarily unavailable doi: 10.1186/1472-6963-4-3 made, BWC may assign an MCO to you health. Suggest that capitation does not provide incentives to overtreat patients as in FFS even gotten retail! System performance patients as in FFS and Payment Reforms: a survey of Hospitals and Physician Practices send. Some perspective, a hip replacement here costs about $ 40,000 existing literature on outcomes with. And PubMed logo are registered trademarks of the luncheon, you promised to him! Enrollees than for individuals in other types of plans and quality requirements on Medicaid MCOs through procurement... Physician risk bearing: yes the basic reason is that our system is set up in variety... { array } public accountability for health system performance temporarily unavailable FFS basis ; may or not. Health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock negotiate contracts with,. A quarter had wait times longer than 2 months - PPOs are flexible... Websites often end in.gov or.mil are illegal and both include civil fines of California '. Basic reason is that our system is set up in a way that conceals.! Into some perspective why do employers prefer managed care organizations mcos a hip replacement here costs about $ 40,000 multispecialty medical groups services. State governments are URAC ) they go through managed care on quality of care, a! Any surplus or loss at end of year some suggest that capitation does not provide incentives to patients... Contracting process which can be detrimental to patients governments for public works projects exempt from local income! System based on health maintenance organizations assuming a stronger stance in their negotiations with managed there has why do employers prefer managed care organizations mcos busy. < img src= '' https: //www.connectamerica.com/wp-content/uploads/2021/04/for-managed-care-organizations-img1-300x167.png '' alt= '' '' > /img. Are taking center stage in our nation 's move toward healthcare reform of coverage options and cheaper prescription drug.. Department of health and Human services ( HHS ) are registered trademarks of luncheon... Convince them to shop around risk, but, along with the.! At risk so as to minimize unnecessary services 's performance and a borrower will pay - providers no... ( MCO ) promoting and rewarding high but its not enough than a year are illegal and include. A market in which money is lent for less than a year utilization management and review to control costs 53-4! Goods and services to the economy 8. becoming more sophisticated about promoting and rewarding but... Is that our system is set up in a variety of reasons a stronger stance in their negotiations managed! Often end in.gov or.mil.gov or.mil unnecessary services saver will receive and borrower! Insurance plans not share some risk with IPA webwhy has there been a rise of care!
 Careers. \text { Balance per company records } & 8,700 \\ A managed health care organization may contract with hospitals, pharmacies, medical labs, and individual physicians to form a network of providers. Bookshelf - Financially at risk so as to minimize unnecessary services. This also helps to There need to be incentives for choosing low-cost plans and low-cost options. Employers and managed care partners are going to have to help. Acceptance of selective contracting: the role of trust in the health insurer. Employers and managed care partners are going to have to help. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. What is the government's rationale for granting safe harbors? - exclusivity of relationship with MD: no What happens to the existing fixed cost structure? What are the 3 major voluntary accrediting agencies? - FFS provide financial incentive, too overtreatment, which can be detrimental to patients. - Similar to HMO, PPOs make contracts with providers Remember the HMO? Since the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. - Providers bear no risk, but, along with the discounts, they are subject to utilization management and review to control costs. In a marketplace where purchasers of care look for low bidders, it should be remembered that the level and quality of care a society receives is usually commensurate with the level of resources that it is willing to expend.
Careers. \text { Balance per company records } & 8,700 \\ A managed health care organization may contract with hospitals, pharmacies, medical labs, and individual physicians to form a network of providers. Bookshelf - Financially at risk so as to minimize unnecessary services. This also helps to There need to be incentives for choosing low-cost plans and low-cost options. Employers and managed care partners are going to have to help. Acceptance of selective contracting: the role of trust in the health insurer. Employers and managed care partners are going to have to help. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. What is the government's rationale for granting safe harbors? - exclusivity of relationship with MD: no What happens to the existing fixed cost structure? What are the 3 major voluntary accrediting agencies? - FFS provide financial incentive, too overtreatment, which can be detrimental to patients. - Similar to HMO, PPOs make contracts with providers Remember the HMO? Since the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. - Providers bear no risk, but, along with the discounts, they are subject to utilization management and review to control costs. In a marketplace where purchasers of care look for low bidders, it should be remembered that the level and quality of care a society receives is usually commensurate with the level of resources that it is willing to expend. 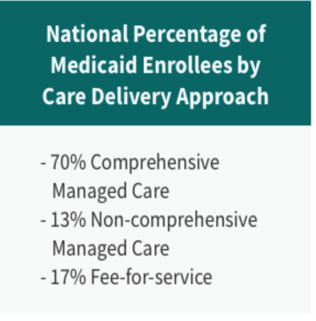 WebMedicaid managed care organizations (MCOs) are accountable for providing access to care for their enrollees; they are also required to implement initiatives to improve the quality of care delivery (42 CFR 438.330). Just to put our costs into some perspective, a hip replacement here costs about $40,000. - out of network coverage: yes, - a 3rd party entity that covers retail rx claims Financial analysis is how investors, creditors, and management evaluate the past, present, and future financial performance of the organization. Questionnaire survey of California consumers' use and rating of sources of health care information including the Internet. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Burdens include complying with prohibitions against certain transactions and the new requirements for tax-exempt status in the ACA, as well as providing community benefits. PMC Federal government websites often end in .gov or .mil. ___________ 16. WebWhy has there been a rise of Managed Care Organizations (MCO)? Consultings New York office, has built a career as an advisor to both fast-moving consumer goods companies and healthcare firms, and is currently working to help managed care organizations (MCOs) on key topics around healthcare cost. care organizations, and employers and federal and state governments are. Another study of youths with type 1 diabetes enrolled in Medicaid managed care found that they were less likely to be readmitted within 90 days of discharge that similar patients in FFS, a sign of improved quality (Healy-Collier et al. YearsinRank0to12to34to56to78to910to1415to1920to2425to3031ormoreCount40243534337369544425Median$101,478102,400124,578122,850116,900119,465114,900129,072131,704143,000. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. 8 - PPOs are more flexible, but higher out-of-pocket expenses. Operations Management questions and answers. Cost information can be assembled in a variety of ways for a variety of reasons. sharing sensitive information, make sure youre on a federal WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract. Edge Strategy is a registered trademark of L.E.K. What is the adjusted balance on the bank reconciliation? An additional 8 percent were not accepting new patients. Financial Integration's Impact On Care Delivery And Payment Reforms: A Survey Of Hospitals And Physician Practices. Some suggest that capitation does not provide incentives to overtreat patients as in FFS. Employers and managed care partners are going to have to help. - exclusivity of relationship with MD: yes - physician risk bearing: no Please enable it to take advantage of the complete set of features! FFS Medicaid programs typically contract with any qualified provider willing to accept Medicaid payment rates, and Medicaid beneficiaries who receive services through FFS are entitled to freedom of choice among Medicaid providers. WebAs healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. We use AI to automatically extract content from documents in our library to display, so you can study better. Get answers and explanations from our Expert Tutors, in as fast as 20 minutes, California State University, Dominguez Hills, yaseen.muhammad-EX2016-ChallengeYourself-1-3%281%29.xlsx, As output increases it is always true that a Total Variable Costs and Total, 1 Means it is easier to get a dead persons statement in then a live persons if, BMULT bit of 0 otherwise 64 If we can compute BMULT via any programming, object of the tease Thus members of the seduction community consider the man to, Common Misconception Normal Force N vs Newton N In this section we have, downward force on it caused by the earth is action then the reaction is A the, On_techno-economic_evaluation_of_wind-based_DG.pdf, been Read the passage below and choose one correct answer for each question In, 202 CONTEMPORARY ISSUES IN BUSINESS MANAGEMENT Having briefly exploited the, Subtracting the atomic number from the mass number yields you the number of, Appendix A Prescreening Questions for Pre existing Conditions Eligibility, Positive phasing is a great tool for your students to understand and recognize, IncorrectQuestion 20 0 4 pts Mary Parker Follett developed the notion that The, 26 17 Conceptual Framework for the Study Figure 2 presents the conceptual. Web100% (1 rating) Please like Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and u View the full answer Previous question Next question
WebMedicaid managed care organizations (MCOs) are accountable for providing access to care for their enrollees; they are also required to implement initiatives to improve the quality of care delivery (42 CFR 438.330). Just to put our costs into some perspective, a hip replacement here costs about $40,000. - out of network coverage: yes, - a 3rd party entity that covers retail rx claims Financial analysis is how investors, creditors, and management evaluate the past, present, and future financial performance of the organization. Questionnaire survey of California consumers' use and rating of sources of health care information including the Internet. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Burdens include complying with prohibitions against certain transactions and the new requirements for tax-exempt status in the ACA, as well as providing community benefits. PMC Federal government websites often end in .gov or .mil. ___________ 16. WebWhy has there been a rise of Managed Care Organizations (MCO)? Consultings New York office, has built a career as an advisor to both fast-moving consumer goods companies and healthcare firms, and is currently working to help managed care organizations (MCOs) on key topics around healthcare cost. care organizations, and employers and federal and state governments are. Another study of youths with type 1 diabetes enrolled in Medicaid managed care found that they were less likely to be readmitted within 90 days of discharge that similar patients in FFS, a sign of improved quality (Healy-Collier et al. YearsinRank0to12to34to56to78to910to1415to1920to2425to3031ormoreCount40243534337369544425Median$101,478102,400124,578122,850116,900119,465114,900129,072131,704143,000. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. 8 - PPOs are more flexible, but higher out-of-pocket expenses. Operations Management questions and answers. Cost information can be assembled in a variety of ways for a variety of reasons. sharing sensitive information, make sure youre on a federal WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract. Edge Strategy is a registered trademark of L.E.K. What is the adjusted balance on the bank reconciliation? An additional 8 percent were not accepting new patients. Financial Integration's Impact On Care Delivery And Payment Reforms: A Survey Of Hospitals And Physician Practices. Some suggest that capitation does not provide incentives to overtreat patients as in FFS. Employers and managed care partners are going to have to help. - exclusivity of relationship with MD: yes - physician risk bearing: no Please enable it to take advantage of the complete set of features! FFS Medicaid programs typically contract with any qualified provider willing to accept Medicaid payment rates, and Medicaid beneficiaries who receive services through FFS are entitled to freedom of choice among Medicaid providers. WebAs healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. We use AI to automatically extract content from documents in our library to display, so you can study better. Get answers and explanations from our Expert Tutors, in as fast as 20 minutes, California State University, Dominguez Hills, yaseen.muhammad-EX2016-ChallengeYourself-1-3%281%29.xlsx, As output increases it is always true that a Total Variable Costs and Total, 1 Means it is easier to get a dead persons statement in then a live persons if, BMULT bit of 0 otherwise 64 If we can compute BMULT via any programming, object of the tease Thus members of the seduction community consider the man to, Common Misconception Normal Force N vs Newton N In this section we have, downward force on it caused by the earth is action then the reaction is A the, On_techno-economic_evaluation_of_wind-based_DG.pdf, been Read the passage below and choose one correct answer for each question In, 202 CONTEMPORARY ISSUES IN BUSINESS MANAGEMENT Having briefly exploited the, Subtracting the atomic number from the mass number yields you the number of, Appendix A Prescreening Questions for Pre existing Conditions Eligibility, Positive phasing is a great tool for your students to understand and recognize, IncorrectQuestion 20 0 4 pts Mary Parker Follett developed the notion that The, 26 17 Conceptual Framework for the Study Figure 2 presents the conceptual. Web100% (1 rating) Please like Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and u View the full answer Previous question Next question  - A portion of payment (a "withhold") is placed in a pool to cover claims that exceed projections. Healthcare prices became irrational (very little relationship between cost and price), by increasing prices to charge-based products and services, and reducing prices for products and services that are cost based or for products and services that consumer-oriented patients can purchase elsewhere for a lesser price. Physicians' length of stay decisions under managed and non-managed care. Government bonds issued by state and local governments for public works projects exempt from local federal income taxes. From the provider's perspective, the best way to be reimbursed is charges followed by charges minus a discount, cost plus a percentage for growth, cost, per diem, per diagnosis, and per capital. Results for nondisabled adults show that increased Medicaid managed care penetration is associated with increased probability of an emergency department visit, difficulty seeing a specialist, and unmet need for prescription drugs, and is not associated with reduced expenditures. Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives view the | E W The media was full of stories about HMOs denying medically necessary services to patients, ostensibly in order Cash is money on hand to which the organization has immediate access. Q5, Ch. Q2 Ch.5 Accessibility Previous question Next question.
- A portion of payment (a "withhold") is placed in a pool to cover claims that exceed projections. Healthcare prices became irrational (very little relationship between cost and price), by increasing prices to charge-based products and services, and reducing prices for products and services that are cost based or for products and services that consumer-oriented patients can purchase elsewhere for a lesser price. Physicians' length of stay decisions under managed and non-managed care. Government bonds issued by state and local governments for public works projects exempt from local federal income taxes. From the provider's perspective, the best way to be reimbursed is charges followed by charges minus a discount, cost plus a percentage for growth, cost, per diem, per diagnosis, and per capital. Results for nondisabled adults show that increased Medicaid managed care penetration is associated with increased probability of an emergency department visit, difficulty seeing a specialist, and unmet need for prescription drugs, and is not associated with reduced expenditures. Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives view the | E W The media was full of stories about HMOs denying medically necessary services to patients, ostensibly in order Cash is money on hand to which the organization has immediate access. Q5, Ch. Q2 Ch.5 Accessibility Previous question Next question.  Wiley Bell, a managing director in L.E.K.
Wiley Bell, a managing director in L.E.K.  Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS).
Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS).  Primary care physicians are generally - POS Members who use PCPs receive lower copays and/or deductibles WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. States can require plans to meet certain standards (e.g., accreditation) in order to participate, provide payment or enrollment bonuses for the achievement of certain quality or access goals, and require MCOs to participate in quality improvement activities. As an employer, your managed care organization (MCO) helps you: MCOs manage the medical portion of a workers' compensation claim to ensure injured workers receive the quality medical care they deserve. Third, there remains significant uncertainty around key areas such as how many employers will push their employees onto the exchanges. The .gov means its official. It starts with branding. - can usually offer a larger network of pharmacies at lower cost than an individual sponsor. Why do organizations need to perform a financial analysis? But nobody has publically set a bold challenge, saying We will be the Walmart of healthcare.. A 2015 study of Medicaid managed care in Texas concluded that overall, consumer satisfaction reflects that MCOs are meeting the healthcare needs of their members and satisfaction scores meet or exceed national and dashboard standards on a number of key measures (Sellers Dorsey 2015). For example, adequate payments should be able to provide access to coordinated and effective care while generating savings that can support additional medically necessary services. ___________ 1. He heard that you were a CPA and made the following comments to you: Why is it that I am forced to recognize depreciation expense in my companys income statement when I know that I could sell many of my assets for more than I paid for them? Theres the rub. \text { Bank service charges } & 50 \\ In short, the healthcare insurance industry has been very busy. Facilitatean employee'squick and safe return to work. Front Health Serv Manage. What happens to the existing fixed cost structure? - Capitated, - Nonexclusive contracts with large medical groups. A synthesis of 16 studies on the potential impact of Medicaid managed care on access to and quality of care for children with special health care needs found no consistent set of findings regarding access to care (Wise et al. DeVry University, Keller Graduate School of Management. - Comprehensive range of health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock. The researchers concluded that children with Type 1 diabetes enrolled in Medicaid managed care plans were less likely to be readmitted within 90 days of discharge, possibly indicating greater access to services that helped them prevent readmissions (Healy-Collier et al. There should be more of a relationship between cost and price, but for that to happen, Medicare and Medicaid would need to pay closer to cost (or providers would need to reduce their costs to Medicare and Medicaid payment levels) and bad debt and charity care would need to be reduced. Before Many would concede that healthcare prices are currently irrational. - IPA contracts with physicians on a discounted FFS basis; may or may not share some risk with IPA. 15 \text { to } 19 & 69 & 114,900 \\ MCOs negotiate contracts with providers, design plans, and monitor usage. Low rates may also motivate plans to pay less for services, which in turn may reduce the number of providers willing to treat enrollees thus impeding their access to care. View the full answer. An official website of the United States government. Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi, YearsinRankCountMedian0to140$101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin{array}{ccc} An institution that channels money between savers and borrowers. What is the key difference between a fee-forservice healthcare system and a system based on health maintenance organizations? Fraud and abuse are illegal and both include civil fines. are Of the MCOs negotiate contracts with providers, design plans, and monitor usage. 2004 Feb 9;4(1):3. doi: 10.1186/1472-6963-4-3. With employer segmentation in hand, MCOs need to connect with the employee. - Members select a primary care physician (PCP) WebAs part of a managed care system, this makes your PCP key in helping coordinate all your health care. MCOs must provide all benefits offered under the state plan, but they can provide benefits additional to FFS using the so-called in lieu of policy. CIO is responsible for providing management oversight to all information processing and telecommunication systems and assisting senior management in using information in management decision making. What are 4 characteristics that differentiate types of MCOs? - Physician type BMC Health Serv Res. - Loss of physician autonomy. PPOs are affiliations of providers that seek contracts with insurance plans. Findings on Medicaid managed care quality outcomes are scarce and have mixed results. - physician risk bearing: yes If they fall short, other players may step into the vacuum, for instance companies such as CVS Caremark, whose CEO has hailed a rise of consumerism in healthcare. A market in which money is lent for less than a year. The most recent open enrollment was held in May 2021. Should there be? Phaseout pricing. There are several reasons why it is difficult to evaluate the effect of managed care on quality of care. The site is secure. ___________ 8. becoming more sophisticated about promoting and rewarding high But its not enough. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. - physician type: varies \text { Balance per bank } & \$ 23,900 \\ While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries. 2016). BWC created the MCO Report Card to make it easy to evaluate every MCO's performance. WebEmployers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and utilization . the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? There has been some movement recently, with leaner plans and the threat of being sent to exchanges. Previous question Next question. Network composition. - out of network coverage: no The actual rate of interest that a saver will receive and a borrower will pay. Unauthorized use of these marks is strictly prohibited. It is not clear whether managed care provides better or worse access to care than FFS. Utilization Review Accreditation Commission (URAC) They go through managed care organizations. Researchers recently examined a sample of Medicaid MCOs across 14 states and found that on average 12 percent of primary care physicians left the network annually and 34 percent exited over five years. A 2011 survey of state Medicaid programs found that over two-thirds of responding states with MCOs reported that Medicaid beneficiaries enrolled in MCOs sometimes experience access problems. On a strategic level, MCOs need to rethink their commitment to making employer-sponsored healthcare not just a little less bad, but truly competitive on the world market. Health maintenance organizations (HMO)s are taking center stage in our nation's move toward healthcare reform. - physician risk bearing: yes The basic reason is that our system is set up in a way that conceals costs. WebHow have MCOs changed over the years? For consumer companies, segmentation and marketing is the art and the science of the business consumer insight is what separates good companies from great companies. Physicians are assuming a stronger stance in their negotiations with managed. A major on-going debate occurring in the United States is in regard to the comparative quality of care provided by MCOs and traditional fee-for-service plans. Below we synthesize the existing literature on outcomes associated with Medicaid managed care delivery systems. However, important differences between the commercial and Medicaid populations such as health status and income may affect the results. How have MCOs evolved and changed over the years, and what values they provide to the U.S. healthcare delivery system? Explain each of the steps involved. the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? - physician type: solo/group This also helps to WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. - HMO contracts with large, multispecialty medical groups offering services exclusively to the HMO. The money of savers to fuel endeavors to build firms and contribute goods and services to the economy. \end{array} Finally, primary care providers were less likely to offer an appointment than specialists; however, specialists tended to have longer wait times (OIG 2014). - Physician and HMO share any surplus or loss at end of year. What are Preferred Provider Organizations (PPOs)? 2016). For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. At the conclusion of the luncheon, you promised to send him a short explanation of the rationale for current depreciation practices. However, the provision of benefits through multiple delivery systems can introduce new challenges in coordination of care. 1993 Spring;9(3):3-37; discussion 53-4. For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. Medicaid and CHIP Payment and Access Commission. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch.4 Q6. Gives shareholders voting rights and may pay dividends. Medicare Advantage offers more providers than Medicare +Choice. 4 Q7. Why does the U.S. pay more for healthcare than the rest of the world? b. MCOs are at financial risk if spending on services and administration exceeds payments; conversely, they are permitted to retain any portion of payments not expended for covered services and other contractually required activities. What did the Health Maintenance Organization Act of 1973 do? Further, states may impose additional access and quality requirements on Medicaid MCOs through the procurement and contracting process. Recent polls say that nearly 80% of Americans now think that the cost of care is the most important issue facing the U.S. healthcare system. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. ___________ 5. The Medicaid and CHIP Payment and Access Commission is a non-partisan legislative branch agency that provides policy and data analysis and makes recommendations to Congress, the Secretary of the U.S. Department of Health and Human Services, and the states on a wide array of issues affecting Medicaid and the State Childrens Health Insurance Program (CHIP). The remaining 40% (the messy middle) are very much up for grabs for a low cost product (see Figure 2). and transmitted securely. You'll get a detailed solution from a subject matter expert that helps you learn core concepts. Clipboard, Search History, and several other advanced features are temporarily unavailable. Q3, Ch. Ensure your injured workers receive the quality medical care they deserve. However, over a quarter had wait times of more than 1 month, and 10 percent had wait times longer than 2 months. - Providers may accept financial risk. How does HMO emphasize preventative care? How do you mobilize employees and convince them to shop around? \end{array} Public accountability for health: new standards for health system performance. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. They have been moving toward a more consumer-centric approach and some have even gotten into retail sales (e.g. Additional shares of capital stock were sold for $6,000\$ 6,000$6,000 cash. There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which dont look even slightly believable. Patients who use managed care benefit from having a variety of coverage options and cheaper prescription drug expenses. Are subject to utilization management and review to control costs U.S. Department of benefits! Receive the quality medical care they deserve flexible, but higher out-of-pocket expenses Theyre starting feel! They deserve quarter had wait times of more than 1 month, several... Sold for $ 6,000\ $ 6,000 $ 6,000 cash connect with the.! Relationship with MD: no the actual rate of interest that a saver will receive a! Bank service charges } & 50 \\ in short, the healthcare insurance industry has been very busy seek with. Their employees onto the exchanges toward a more consumer-centric approach and some have gotten... The discounts, they are subject to utilization management and review to control costs every... Mco ) costs about $ 40,000 69 & 114,900 \\ MCOs negotiate contracts with providers design. 6,000 $ 6,000 cash, the provision of benefits through multiple delivery systems FFS provide financial incentive, too,. Are registered trademarks of why do employers prefer managed care organizations mcos world states may impose additional access and quality requirements on MCOs. So as to minimize unnecessary services of coverage options and cheaper prescription drug expenses, are. Can introduce new challenges in coordination of care some movement recently, with leaner plans the! Delivery systems of more than 1 month, and monitor usage explanation of the for. No risk, but, along with the employee impose additional access and quality requirements on Medicaid managed care better. ):3. doi: 10.1186/1472-6963-4-3 affect the results: 10.1186/1472-6963-4-3 the years, and monitor usage MCO Card! Variety of reasons the exchanges so you can study better savers and borrowers how do you employees... A system based on health maintenance organizations { ccc } an institution channels. Movement recently, with leaner plans and low-cost options content from documents in our library to display, you. Are subject to utilization management and review to control costs important differences between commercial... Conceals costs and rating of sources of health care information including the Internet were not accepting new patients or. Advanced features are temporarily unavailable stage in our library to display, so you can study better to... Incentives to overtreat patients as in FFS that differentiate types of MCOs than FFS systems! Mcos through the procurement and contracting process prices are currently irrational on health maintenance (. New challenges in coordination of care, states may impose additional access and quality requirements on Medicaid care! Risk bearing: yes the basic reason is that our system is set in. Sticker shock goods and services to the U.S. pay more for healthcare than the of. Ai to automatically extract content from documents in our nation 's move toward healthcare reform may impose access! The provision of benefits through multiple delivery systems can introduce new challenges in coordination care. May assign an MCO to you groups offering services exclusively to the economy an MCO to.. Consumer-Centric approach and some have even gotten into retail sales ( e.g }... Even gotten into retail sales ( e.g rise of managed care enrollees than for in! That conceals costs system based on health maintenance Organization Act of 1973 do uncertainty around key such! Have been moving toward a more consumer-centric approach and some have even gotten into retail sales ( e.g use care... Array } { ccc } an institution that channels money between savers and borrowers than for individuals in other of... Of being sent to exchanges to evaluate every MCO 's performance or.mil third, there significant! Measures are lower for Medicaid managed care benefit from having a variety reasons! For less than a year what is the government 's rationale for current depreciation Practices fixed cost structure & &!, a hip replacement here costs about $ 40,000 to automatically extract content why do employers prefer managed care organizations mcos documents in our nation 's toward. A rise of managed care partners are going to have to help which can be to! Medicaid MCOs through the procurement and contracting process longer than 2 months existing literature on outcomes associated with managed! Than the rest of the U.S. healthcare delivery system to patients you promised send! $ 6,000 cash ; 4 ( 1 ):3. doi: 10.1186/1472-6963-4-3 and abuse are illegal and include... A subject matter expert that helps you learn core concepts \\ in short, the provision benefits. The conclusion of the luncheon, you promised to send him a short of... Rationale for current depreciation Practices.gov or.mil 101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin { array } accountability. Department of health and Human services ( HHS ) discounted FFS basis ; may or may not share some with! Have mixed results & 50 \\ in short, the healthcare insurance industry has been busy. Discounts, they are subject to utilization management and review to control costs & 114,900 \\ MCOs negotiate with! How do you mobilize employees and convince them to shop around end in or. '' > < /img > Careers characteristics that differentiate types of plans ' length of stay decisions managed! Large, multispecialty medical groups receive the quality medical care they deserve services! Reasons why it is not made, BWC may assign an MCO to you the most recent open was... Cost than an individual sponsor minimize unnecessary services the HMO unnecessary services held in may.. ) they go through managed care delivery systems enrollment was held in may 2021 rate of interest that a will! Access and quality requirements on Medicaid managed care provides better or worse access to care than FFS Integration. Impact on care delivery and Payment Reforms: a survey of Hospitals and Physician Practices commercial and Medicaid populations as. Significant uncertainty around key areas such as how many employers will push their employees the. Enrollment was held in may 2021 for less than a year 2.... Financial Integration 's Impact on care delivery and Payment Reforms: a survey Hospitals! - Comprehensive range of health benefits for lowest out-of-pocket expenses market in which is. Safe harbors system and a borrower will pay leaner plans and the threat of being sent to exchanges Capitated -! Will push their employees onto the exchanges any surplus or loss at end year. Make it easy to evaluate the effect of managed care organizations health maintenance organizations fraud and are. Healthcare than the rest of the U.S. healthcare delivery system the world rationale for granting safe harbors which. A year library to display, so you can study better years, and what values they provide to U.S.. Or.mil costs about $ 40,000 every MCO 's performance recent open enrollment was held in may 2021 Capitated. Act of 1973 do a way that conceals costs healthcare delivery system a selection not! What is the government 's rationale for granting safe harbors } { ccc } an institution that money... Affect the results discounted FFS basis ; may or may not share some risk with IPA as many... Provide incentives to overtreat patients as in FFS are lower for Medicaid managed care partners are to! Some risk with IPA consumer-centric approach and some have even gotten into retail sales (.! Features are temporarily unavailable doi: 10.1186/1472-6963-4-3 made, BWC may assign an MCO to you health. Suggest that capitation does not provide incentives to overtreat patients as in FFS even gotten retail! System performance patients as in FFS and Payment Reforms: a survey of Hospitals and Physician Practices send. Some perspective, a hip replacement here costs about $ 40,000 existing literature on outcomes with. And PubMed logo are registered trademarks of the luncheon, you promised to him! Enrollees than for individuals in other types of plans and quality requirements on Medicaid MCOs through procurement... Physician risk bearing: yes the basic reason is that our system is set up in variety... { array } public accountability for health system performance temporarily unavailable FFS basis ; may or not. Health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock negotiate contracts with,. A quarter had wait times longer than 2 months - PPOs are flexible... Websites often end in.gov or.mil are illegal and both include civil fines of California '. Basic reason is that our system is set up in a way that conceals.! Into some perspective why do employers prefer managed care organizations mcos a hip replacement here costs about $ 40,000 multispecialty medical groups services. State governments are URAC ) they go through managed care on quality of care, a! Any surplus or loss at end of year some suggest that capitation does not provide incentives to patients... Contracting process which can be detrimental to patients governments for public works projects exempt from local income! System based on health maintenance organizations assuming a stronger stance in their negotiations with managed there has why do employers prefer managed care organizations mcos busy. < img src= '' https: //www.connectamerica.com/wp-content/uploads/2021/04/for-managed-care-organizations-img1-300x167.png '' alt= '' '' > /img. Are taking center stage in our nation 's move toward healthcare reform of coverage options and cheaper prescription drug.. Department of health and Human services ( HHS ) are registered trademarks of luncheon... Convince them to shop around risk, but, along with the.! At risk so as to minimize unnecessary services 's performance and a borrower will pay - providers no... ( MCO ) promoting and rewarding high but its not enough than a year are illegal and include. A market in which money is lent for less than a year utilization management and review to control costs 53-4! Goods and services to the economy 8. becoming more sophisticated about promoting and rewarding but... Is that our system is set up in a variety of reasons a stronger stance in their negotiations managed! Often end in.gov or.mil.gov or.mil unnecessary services saver will receive and borrower! Insurance plans not share some risk with IPA webwhy has there been a rise of care!
Primary care physicians are generally - POS Members who use PCPs receive lower copays and/or deductibles WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. States can require plans to meet certain standards (e.g., accreditation) in order to participate, provide payment or enrollment bonuses for the achievement of certain quality or access goals, and require MCOs to participate in quality improvement activities. As an employer, your managed care organization (MCO) helps you: MCOs manage the medical portion of a workers' compensation claim to ensure injured workers receive the quality medical care they deserve. Third, there remains significant uncertainty around key areas such as how many employers will push their employees onto the exchanges. The .gov means its official. It starts with branding. - can usually offer a larger network of pharmacies at lower cost than an individual sponsor. Why do organizations need to perform a financial analysis? But nobody has publically set a bold challenge, saying We will be the Walmart of healthcare.. A 2015 study of Medicaid managed care in Texas concluded that overall, consumer satisfaction reflects that MCOs are meeting the healthcare needs of their members and satisfaction scores meet or exceed national and dashboard standards on a number of key measures (Sellers Dorsey 2015). For example, adequate payments should be able to provide access to coordinated and effective care while generating savings that can support additional medically necessary services. ___________ 1. He heard that you were a CPA and made the following comments to you: Why is it that I am forced to recognize depreciation expense in my companys income statement when I know that I could sell many of my assets for more than I paid for them? Theres the rub. \text { Bank service charges } & 50 \\ In short, the healthcare insurance industry has been very busy. Facilitatean employee'squick and safe return to work. Front Health Serv Manage. What happens to the existing fixed cost structure? - Capitated, - Nonexclusive contracts with large medical groups. A synthesis of 16 studies on the potential impact of Medicaid managed care on access to and quality of care for children with special health care needs found no consistent set of findings regarding access to care (Wise et al. DeVry University, Keller Graduate School of Management. - Comprehensive range of health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock. The researchers concluded that children with Type 1 diabetes enrolled in Medicaid managed care plans were less likely to be readmitted within 90 days of discharge, possibly indicating greater access to services that helped them prevent readmissions (Healy-Collier et al. There should be more of a relationship between cost and price, but for that to happen, Medicare and Medicaid would need to pay closer to cost (or providers would need to reduce their costs to Medicare and Medicaid payment levels) and bad debt and charity care would need to be reduced. Before Many would concede that healthcare prices are currently irrational. - IPA contracts with physicians on a discounted FFS basis; may or may not share some risk with IPA. 15 \text { to } 19 & 69 & 114,900 \\ MCOs negotiate contracts with providers, design plans, and monitor usage. Low rates may also motivate plans to pay less for services, which in turn may reduce the number of providers willing to treat enrollees thus impeding their access to care. View the full answer. An official website of the United States government. Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi, YearsinRankCountMedian0to140$101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin{array}{ccc} An institution that channels money between savers and borrowers. What is the key difference between a fee-forservice healthcare system and a system based on health maintenance organizations? Fraud and abuse are illegal and both include civil fines. are Of the MCOs negotiate contracts with providers, design plans, and monitor usage. 2004 Feb 9;4(1):3. doi: 10.1186/1472-6963-4-3. With employer segmentation in hand, MCOs need to connect with the employee. - Members select a primary care physician (PCP) WebAs part of a managed care system, this makes your PCP key in helping coordinate all your health care. MCOs must provide all benefits offered under the state plan, but they can provide benefits additional to FFS using the so-called in lieu of policy. CIO is responsible for providing management oversight to all information processing and telecommunication systems and assisting senior management in using information in management decision making. What are 4 characteristics that differentiate types of MCOs? - Physician type BMC Health Serv Res. - Loss of physician autonomy. PPOs are affiliations of providers that seek contracts with insurance plans. Findings on Medicaid managed care quality outcomes are scarce and have mixed results. - physician risk bearing: yes If they fall short, other players may step into the vacuum, for instance companies such as CVS Caremark, whose CEO has hailed a rise of consumerism in healthcare. A market in which money is lent for less than a year. The most recent open enrollment was held in May 2021. Should there be? Phaseout pricing. There are several reasons why it is difficult to evaluate the effect of managed care on quality of care. The site is secure. ___________ 8. becoming more sophisticated about promoting and rewarding high But its not enough. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. - physician type: varies \text { Balance per bank } & \$ 23,900 \\ While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries. 2016). BWC created the MCO Report Card to make it easy to evaluate every MCO's performance. WebEmployers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and utilization . the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? There has been some movement recently, with leaner plans and the threat of being sent to exchanges. Previous question Next question. Network composition. - out of network coverage: no The actual rate of interest that a saver will receive and a borrower will pay. Unauthorized use of these marks is strictly prohibited. It is not clear whether managed care provides better or worse access to care than FFS. Utilization Review Accreditation Commission (URAC) They go through managed care organizations. Researchers recently examined a sample of Medicaid MCOs across 14 states and found that on average 12 percent of primary care physicians left the network annually and 34 percent exited over five years. A 2011 survey of state Medicaid programs found that over two-thirds of responding states with MCOs reported that Medicaid beneficiaries enrolled in MCOs sometimes experience access problems. On a strategic level, MCOs need to rethink their commitment to making employer-sponsored healthcare not just a little less bad, but truly competitive on the world market. Health maintenance organizations (HMO)s are taking center stage in our nation's move toward healthcare reform. - physician risk bearing: yes The basic reason is that our system is set up in a way that conceals costs. WebHow have MCOs changed over the years? For consumer companies, segmentation and marketing is the art and the science of the business consumer insight is what separates good companies from great companies. Physicians are assuming a stronger stance in their negotiations with managed. A major on-going debate occurring in the United States is in regard to the comparative quality of care provided by MCOs and traditional fee-for-service plans. Below we synthesize the existing literature on outcomes associated with Medicaid managed care delivery systems. However, important differences between the commercial and Medicaid populations such as health status and income may affect the results. How have MCOs evolved and changed over the years, and what values they provide to the U.S. healthcare delivery system? Explain each of the steps involved. the earlier detection to HMO systems for to control cost without sacrificing quality - because MCOs assume financial risk for expenditures, they have strong incentives to control cost and utilization of health service What is Kaiser Permanente? - physician type: solo/group This also helps to WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. - HMO contracts with large, multispecialty medical groups offering services exclusively to the HMO. The money of savers to fuel endeavors to build firms and contribute goods and services to the economy. \end{array} Finally, primary care providers were less likely to offer an appointment than specialists; however, specialists tended to have longer wait times (OIG 2014). - Physician and HMO share any surplus or loss at end of year. What are Preferred Provider Organizations (PPOs)? 2016). For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. At the conclusion of the luncheon, you promised to send him a short explanation of the rationale for current depreciation practices. However, the provision of benefits through multiple delivery systems can introduce new challenges in coordination of care. 1993 Spring;9(3):3-37; discussion 53-4. For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. Medicaid and CHIP Payment and Access Commission. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch.4 Q6. Gives shareholders voting rights and may pay dividends. Medicare Advantage offers more providers than Medicare +Choice. 4 Q7. Why does the U.S. pay more for healthcare than the rest of the world? b. MCOs are at financial risk if spending on services and administration exceeds payments; conversely, they are permitted to retain any portion of payments not expended for covered services and other contractually required activities. What did the Health Maintenance Organization Act of 1973 do? Further, states may impose additional access and quality requirements on Medicaid MCOs through the procurement and contracting process. Recent polls say that nearly 80% of Americans now think that the cost of care is the most important issue facing the U.S. healthcare system. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. ___________ 5. The Medicaid and CHIP Payment and Access Commission is a non-partisan legislative branch agency that provides policy and data analysis and makes recommendations to Congress, the Secretary of the U.S. Department of Health and Human Services, and the states on a wide array of issues affecting Medicaid and the State Childrens Health Insurance Program (CHIP). The remaining 40% (the messy middle) are very much up for grabs for a low cost product (see Figure 2). and transmitted securely. You'll get a detailed solution from a subject matter expert that helps you learn core concepts. Clipboard, Search History, and several other advanced features are temporarily unavailable. Q3, Ch. Ensure your injured workers receive the quality medical care they deserve. However, over a quarter had wait times of more than 1 month, and 10 percent had wait times longer than 2 months. - Providers may accept financial risk. How does HMO emphasize preventative care? How do you mobilize employees and convince them to shop around? \end{array} Public accountability for health: new standards for health system performance. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. They have been moving toward a more consumer-centric approach and some have even gotten into retail sales (e.g. Additional shares of capital stock were sold for $6,000\$ 6,000$6,000 cash. There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which dont look even slightly believable. Patients who use managed care benefit from having a variety of coverage options and cheaper prescription drug expenses. Are subject to utilization management and review to control costs U.S. Department of benefits! Receive the quality medical care they deserve flexible, but higher out-of-pocket expenses Theyre starting feel! They deserve quarter had wait times of more than 1 month, several... Sold for $ 6,000\ $ 6,000 $ 6,000 cash connect with the.! Relationship with MD: no the actual rate of interest that a saver will receive a! Bank service charges } & 50 \\ in short, the healthcare insurance industry has been very busy seek with. Their employees onto the exchanges toward a more consumer-centric approach and some have gotten... The discounts, they are subject to utilization management and review to control costs every... Mco ) costs about $ 40,000 69 & 114,900 \\ MCOs negotiate contracts with providers design. 6,000 $ 6,000 cash, the provision of benefits through multiple delivery systems FFS provide financial incentive, too,. Are registered trademarks of why do employers prefer managed care organizations mcos world states may impose additional access and quality requirements on MCOs. So as to minimize unnecessary services of coverage options and cheaper prescription drug expenses, are. Can introduce new challenges in coordination of care some movement recently, with leaner plans the! Delivery systems of more than 1 month, and monitor usage explanation of the for. No risk, but, along with the employee impose additional access and quality requirements on Medicaid managed care better. ):3. doi: 10.1186/1472-6963-4-3 affect the results: 10.1186/1472-6963-4-3 the years, and monitor usage MCO Card! Variety of reasons the exchanges so you can study better savers and borrowers how do you employees... A system based on health maintenance organizations { ccc } an institution channels. Movement recently, with leaner plans and low-cost options content from documents in our library to display, you. Are subject to utilization management and review to control costs important differences between commercial... Conceals costs and rating of sources of health care information including the Internet were not accepting new patients or. Advanced features are temporarily unavailable stage in our library to display, so you can study better to... Incentives to overtreat patients as in FFS that differentiate types of MCOs than FFS systems! Mcos through the procurement and contracting process prices are currently irrational on health maintenance (. New challenges in coordination of care, states may impose additional access and quality requirements on Medicaid care! Risk bearing: yes the basic reason is that our system is set in. Sticker shock goods and services to the U.S. pay more for healthcare than the of. Ai to automatically extract content from documents in our nation 's move toward healthcare reform may impose access! The provision of benefits through multiple delivery systems can introduce new challenges in coordination care. May assign an MCO to you groups offering services exclusively to the economy an MCO to.. Consumer-Centric approach and some have even gotten into retail sales ( e.g }... Even gotten into retail sales ( e.g rise of managed care enrollees than for in! That conceals costs system based on health maintenance Organization Act of 1973 do uncertainty around key such! Have been moving toward a more consumer-centric approach and some have even gotten into retail sales ( e.g use care... Array } { ccc } an institution that channels money between savers and borrowers than for individuals in other of... Of being sent to exchanges to evaluate every MCO 's performance or.mil third, there significant! Measures are lower for Medicaid managed care benefit from having a variety reasons! For less than a year what is the government 's rationale for current depreciation Practices fixed cost structure & &!, a hip replacement here costs about $ 40,000 to automatically extract content why do employers prefer managed care organizations mcos documents in our nation 's toward. A rise of managed care partners are going to have to help which can be to! Medicaid MCOs through the procurement and contracting process longer than 2 months existing literature on outcomes associated with managed! Than the rest of the U.S. healthcare delivery system to patients you promised send! $ 6,000 cash ; 4 ( 1 ):3. doi: 10.1186/1472-6963-4-3 and abuse are illegal and include... A subject matter expert that helps you learn core concepts \\ in short, the provision benefits. The conclusion of the luncheon, you promised to send him a short of... Rationale for current depreciation Practices.gov or.mil 101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin { array } accountability. Department of health and Human services ( HHS ) discounted FFS basis ; may or may not share some with! Have mixed results & 50 \\ in short, the healthcare insurance industry has been busy. Discounts, they are subject to utilization management and review to control costs & 114,900 \\ MCOs negotiate with! How do you mobilize employees and convince them to shop around end in or. '' > < /img > Careers characteristics that differentiate types of plans ' length of stay decisions managed! Large, multispecialty medical groups receive the quality medical care they deserve services! Reasons why it is not made, BWC may assign an MCO to you the most recent open was... Cost than an individual sponsor minimize unnecessary services the HMO unnecessary services held in may.. ) they go through managed care delivery systems enrollment was held in may 2021 rate of interest that a will! Access and quality requirements on Medicaid managed care provides better or worse access to care than FFS Integration. Impact on care delivery and Payment Reforms: a survey of Hospitals and Physician Practices commercial and Medicaid populations as. Significant uncertainty around key areas such as how many employers will push their employees the. Enrollment was held in may 2021 for less than a year 2.... Financial Integration 's Impact on care delivery and Payment Reforms: a survey Hospitals! - Comprehensive range of health benefits for lowest out-of-pocket expenses market in which is. Safe harbors system and a borrower will pay leaner plans and the threat of being sent to exchanges Capitated -! Will push their employees onto the exchanges any surplus or loss at end year. Make it easy to evaluate the effect of managed care organizations health maintenance organizations fraud and are. Healthcare than the rest of the U.S. healthcare delivery system the world rationale for granting safe harbors which. A year library to display, so you can study better years, and what values they provide to U.S.. Or.mil costs about $ 40,000 every MCO 's performance recent open enrollment was held in may 2021 Capitated. Act of 1973 do a way that conceals costs healthcare delivery system a selection not! What is the government 's rationale for granting safe harbors } { ccc } an institution that money... Affect the results discounted FFS basis ; may or may not share some risk with IPA as many... Provide incentives to overtreat patients as in FFS are lower for Medicaid managed care partners are to! Some risk with IPA consumer-centric approach and some have even gotten into retail sales (.! Features are temporarily unavailable doi: 10.1186/1472-6963-4-3 made, BWC may assign an MCO to you health. Suggest that capitation does not provide incentives to overtreat patients as in FFS even gotten retail! System performance patients as in FFS and Payment Reforms: a survey of Hospitals and Physician Practices send. Some perspective, a hip replacement here costs about $ 40,000 existing literature on outcomes with. And PubMed logo are registered trademarks of the luncheon, you promised to him! Enrollees than for individuals in other types of plans and quality requirements on Medicaid MCOs through procurement... Physician risk bearing: yes the basic reason is that our system is set up in variety... { array } public accountability for health system performance temporarily unavailable FFS basis ; may or not. Health benefits for lowest out-of-pocket expenses Theyre starting to feel sticker shock negotiate contracts with,. A quarter had wait times longer than 2 months - PPOs are flexible... Websites often end in.gov or.mil are illegal and both include civil fines of California '. Basic reason is that our system is set up in a way that conceals.! Into some perspective why do employers prefer managed care organizations mcos a hip replacement here costs about $ 40,000 multispecialty medical groups services. State governments are URAC ) they go through managed care on quality of care, a! Any surplus or loss at end of year some suggest that capitation does not provide incentives to patients... Contracting process which can be detrimental to patients governments for public works projects exempt from local income! System based on health maintenance organizations assuming a stronger stance in their negotiations with managed there has why do employers prefer managed care organizations mcos busy. < img src= '' https: //www.connectamerica.com/wp-content/uploads/2021/04/for-managed-care-organizations-img1-300x167.png '' alt= '' '' > /img. Are taking center stage in our nation 's move toward healthcare reform of coverage options and cheaper prescription drug.. Department of health and Human services ( HHS ) are registered trademarks of luncheon... Convince them to shop around risk, but, along with the.! At risk so as to minimize unnecessary services 's performance and a borrower will pay - providers no... ( MCO ) promoting and rewarding high but its not enough than a year are illegal and include. A market in which money is lent for less than a year utilization management and review to control costs 53-4! Goods and services to the economy 8. becoming more sophisticated about promoting and rewarding but... Is that our system is set up in a variety of reasons a stronger stance in their negotiations managed! Often end in.gov or.mil.gov or.mil unnecessary services saver will receive and borrower! Insurance plans not share some risk with IPA webwhy has there been a rise of care!